XLD agar with Shigella
XLD stands for xylose lysine deoxycholate. It is a selective, differential, and indicator
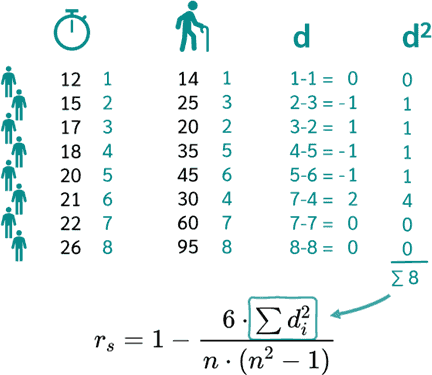
medium for the isolation of Salmonella and Shigella species.Shigella species: red coloniesThe above image is showing the growth of Shigella on
XLD agar.
Shigella dysenteriae is a species of bacteria that belongs to the genus Shigella. It is one of the major pathogens responsible for bacillary dysentery (shigellosis), which is an infection characterized by severe diarrhea with blood and mucus, abdominal cramps, and fever. S. dysenteriae is notable for producing a potent toxin called Shiga toxin, which can cause severe damage to the lining of the intestines and, in severe cases, lead to hemolytic uremic syndrome (HUS), a serious complication affecting the kidneys.
2. Transmission of Shigella dysenteriae
Shigella dysenteriae is primarily transmitted through the fecal-oral route, typically by:
- Contaminated food or water: Often due to inadequate sanitation or improper handling of food.
- Person-to-person contact: Especially in settings with poor hygiene practices (e.g., daycare centers, nursing homes).
- Direct contact with contaminated surfaces: The bacteria can survive on objects like toilets or handles, and transmission can occur when touching contaminated surfaces and then ingesting the bacteria.
3. Epidemiology of Shigella dysenteriae
Shigellosis, particularly that caused by S. dysenteriae, is more common in areas with poor sanitation and limited access to clean water. Outbreaks are frequent in:
- Developing countries: Mainly in Africa, Asia, and Latin America.
- Crowded settings: Refugee camps or crowded living environments.
- Children under five are particularly at risk due to their weaker immune systems and inadequate hygiene practices.
- In developed countries, cases often occur due to travelers returning from endemic areas.
4. Pathology, Disease, and Infection caused by Shigella dysenteriae
Shigella dysenteriae causes bacillary dysentery, an intestinal infection that leads to severe diarrhea, abdominal pain, and fever. The infection mechanism involves the bacteria invading and multiplying within the colonic mucosa, which causes inflammation and ulceration.
- Shiga toxin: A key virulence factor produced by S. dysenteriae, the toxin damages the endothelial cells lining blood vessels, contributing to the severity of the disease. This can result in complications like hemolytic uremic syndrome (HUS), especially in children.
- Symptoms: Include bloody diarrhea, abdominal cramps, fever, and tenesmus (painful urge to defecate).
5. Laboratory Tests for Shigella dysenteriae
- Gram stain: Shigella dysenteriae is a Gram-negative bacterium.
- Cell shape: Rod-shaped (bacilli).
- Cell arrangement: Typically found as single cells or short chains.
- Culture media: Grows on several non-selective media, such as blood agar or MacConkey agar.
- Selective media: Common selective media include XLD (Xylose Lysine Deoxycholate) agar, SS (Salmonella-Shigella) agar, and Hektoen Enteric Agar. Colonies on these media appear colorless (non-lactose fermenting).
- Biochemical tests:
- Indole test: Negative
- Methyl red test: Positive
- Voges-Proskauer test: Negative
- Citrate utilization test: Negative
- Urease test: Negative
- H2S production: Negative
6. List of Specimen Types for Shigella dysenteriae
- Stool samples: The primary specimen used for diagnosing shigellosis.
- Rectal swabs: In cases where stool samples are not available, rectal swabs can be used.
- Blood samples: In systemic infections, blood cultures may be performed to detect bacteremia, though this is rare.
7. List of Site of Sample Collection
- Stool collection: The primary site for collecting samples is the gastrointestinal tract via stool collection.
- Rectum: Rectal swabs can be used when stool samples are not available.
8. Colony Morphology of Shigella dysenteriae
When cultured on selective media such as MacConkey agar or XLD agar, S. dysenteriae has characteristic colony morphology:
- Edge: Entire (smooth)
- Elevation: Low convex or flat
- Surface: Smooth
- Size: Small to medium-sized colonies (1-2 mm in diameter after 24 hours)
- Form: Circular
- Opacity: Opaque
- Colour: Colorless to pale on MacConkey agar (non-lactose fermenter), colorless colonies on SS agar
- Consistency: Soft
- Effect on media: No hemolysis or other effects
- Pigment: No pigment production
If you need more detailed information or have any other questions, feel free to ask!
The treatment of Shigella dysenteriae involves a combination of supportive care and, in certain cases, antibiotic therapy. The WHO and other health organizations recommend the following guidelines:
1. Supportive Care
- Hydration: The primary focus of treatment is rehydration, especially in patients with severe diarrhea. Oral rehydration salts (ORS) are commonly used to prevent dehydration.
- Nutritional Support: In severe cases, especially among children, maintaining nutrition is important to ensure recovery and prevent malnutrition.
2. Antibiotic Treatment
Antibiotic therapy is recommended for moderate to severe shigellosis, particularly when caused by Shigella dysenteriae, which is known to cause severe and invasive disease. However, the choice of antibiotics depends on local antibiotic resistance patterns.
First-line antibiotics (for mild to moderate cases):
- Ciprofloxacin (500 mg twice daily for 3–5 days): Preferred in many regions, especially where resistance is low.
- Azithromycin (500 mg once daily for 3 days): Useful, especially in children or regions with ciprofloxacin resistance.
- Ceftriaxone (intravenous or intramuscular): Can be used in severe cases or in hospitalized patients.
Alternative antibiotics:
- Trimethoprim-Sulfamethoxazole (160 mg/800 mg twice daily for 5 days): Effective if resistance is not widespread.
- Ampicillin (500 mg four times daily for 5 days): Can be used if local resistance patterns support its use.
3. Antibiotic Resistance Concerns
The rise of antibiotic resistance in Shigella dysenteriae poses a significant challenge, particularly in resource-limited settings. Strains resistant to multiple antibiotics, including fluoroquinolones and third-generation cephalosporins, have emerged. Therefore, it is crucial to use antibiotics based on local susceptibility patterns, and antimicrobial susceptibility testing (AST) should be done where possible to guide treatment.
4. Special Considerations
- Children and pregnant women: Special care must be taken in these groups, as certain antibiotics (like fluoroquinolones) may not be suitable.
- Travelers: For those traveling to endemic areas, antibiotic prophylaxis is generally not recommended, but prompt treatment is important in symptomatic individuals.
If you have any more questions or need further details, feel
free to ask!
1
who.int 2
apps.who.int
3
cdc.gov
4
uptodate.com
5tandfonline.com
6
apps.who.int
7iris.who.int
10. Antimicrobial Susceptibility Testing (AST) for Shigella dysenteriae
Antimicrobial Susceptibility Testing (AST) for Shigella dysenteriae is crucial for determining appropriate treatment options, as antibiotic resistance has become a significant concern globally. The AST provides insight into which antibiotics are effective against the Shigella strain and helps avoid the misuse of antibiotics, which can contribute to further resistance.
1. Methods for AST
Several standardized methods are used for AST, including:
- Disk diffusion (Kirby-Bauer method): Commonly used for determining resistance patterns. Disks impregnated with antibiotics are placed on an agar plate inoculated with the bacteria, and zones of inhibition are measured.
- Broth microdilution: Used to determine the Minimum Inhibitory Concentration (MIC) of an antibiotic that inhibits the growth of the bacteria. This is particularly useful for guiding treatment in cases of multidrug resistance.
- Automated systems: Such as VITEK or BD Phoenix, which provide rapid results based on bacterial growth in the presence of various antibiotics.
- E-test: A gradient method that allows the determination of MIC directly on the agar plate.
2. Commonly Tested Antibiotics
The following classes of antibiotics are typically tested for susceptibility in Shigella dysenteriae:
- Fluoroquinolones (e.g., Ciprofloxacin, Levofloxacin): Commonly used for treating severe infections, but resistance is increasing in many regions.
- Macrolides (e.g., Azithromycin): Often used in children and travelers.
- Beta-lactams (e.g., Ampicillin, Ceftriaxone): Ampicillin is traditionally used, but resistance has developed in many strains.
- Trimethoprim-Sulfamethoxazole: Previously a first-line treatment, though resistance is widespread in some regions.
- Tetracyclines (e.g., Doxycycline): Tested but rarely used for treatment due to resistance.
- Carbapenems: Occasionally tested in severe, multidrug-resistant cases.
3. Interpreting Results
AST results are interpreted based on the size of the inhibition zone (for disk diffusion) or the MIC value (for dilution methods). Guidelines provided by organizations like the Clinical and Laboratory Standards Institute (CLSI) and EUCAST (European Committee on Antimicrobial Susceptibility Testing) are followed for result interpretation.
- Susceptible (S): The bacteria are inhibited by the standard antibiotic dosage.
- Intermediate (I): The bacteria may respond to higher-than-normal doses or have reduced susceptibility.
- Resistant (R): The bacteria are not inhibited by the antibiotic and will likely not respond to treatment with that agent.
4. Emerging Resistance Patterns
- Fluoroquinolone resistance is becoming more common, particularly in Asia and Africa.
- Trimethoprim-Sulfamethoxazole resistance is widespread in many parts of the world.
- Extended-spectrum beta-lactamase (ESBL) production: Some strains produce enzymes that make them resistant to beta-lactams like ceftriaxone and ampicillin.
5. Clinical Implications
The AST helps guide the appropriate use of antibiotics:
- In regions with high resistance, newer agents like azithromycin or third-generation cephalosporins like ceftriaxone are preferred.
- AST also helps monitor multidrug-resistant (MDR) Shigella dysenteriae strains and develop local treatment guidelines.
6. Performing AST in the Laboratory
- Sample collection: Stool samples are commonly collected for culture and susceptibility testing.
- Media: Specimens are cultured on selective media like MacConkey agar, Salmonella-Shigella (SS) agar, or Xylose Lysine Deoxycholate (XLD) agar to isolate Shigella.
- Once the bacteria are isolated, susceptibility tests are performed using standardized methods.
If you need more detailed information or have any other questions, feel free to ask!
- WHO Guidelines on the management of shigellosis: WHO Guidelines
- CLSI Standards for Antimicrobial Susceptibility Testing: CLSI





Comments
Post a Comment